Growing older is already a complex process. Dealing with health insurance denials can make things even worse!
A health insurance denial happens when your company refuses to pay for something. If this occurs after you’ve had a medical service and your claim has been submitted, it’s called a claim denial. The entire process can be pretty confusing.
That’s why Easy Seniors Club has discovered all the ins and outs of navigating the intricacies of health insurance denials. We wish to shed some light on common pitfalls that could leave you without coverage when you need it the most.
We’ll also try to provide you with practical solutions and the knowledge to advocate for yourself effectively. A health plan can deny payment for a healthcare service for many reasons. Some are simple and relatively easy to fix, while others are more difficult to address.
Whether it’s misunderstood policies, overlooked paperwork, or any other challenges, understanding these factors is vital to securing the coverage you deserve.
Continue reading to learn some more about the reasons for 7 health insurance denials and empower yourself with the tools to navigate your golden years confidently.

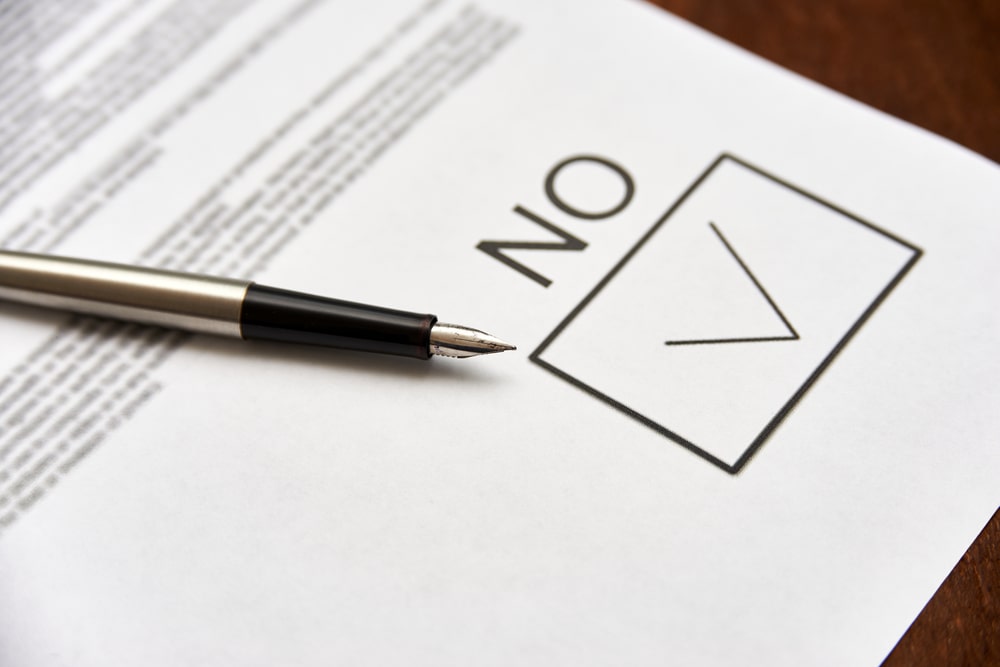
You wrote the incorrect information on your application
Insurers are permitted to deny an application based on incorrect information. An insurer will generally do a background check and look into medical records to ensure the applicant isn’t fabricating information on their application.
In most states insurers can legally deny an applicant solely based on incorrect information filled in on their forms. But, in the state of California, insurers can only reject someone based on wrong information that could affect any future medical care.
For instance, if someone with hazel eyes puts their eye color down as blue, it won’t result in a health insurance denial on this basis alone.
You didn’t pay your premiums on a previous policy
Some applications can lead to health insurance denials due to non-paying premiums from a previous health insurance plan. This case is especially true if they’ve had a previous policy canceled due to non-payment and are applying for a new one with the same insurer.
Those in this position should apply through another insurance company because they’ll have a better chance of getting approval. But their acceptance isn’t necessarily guaranteed.
Some insurance companies will investigate and find out if there are any collections accounts due to the non-payment of health insurance premiums and can deny an applicant based on this criteria.
A Grandfathered Plan can result in health insurance denial based on pre-existing conditions
A plan bought before March 2010 is grandfathered under the Affordable Care Act. Someone can still be denied a renewal of this plan if they have a pre-existing condition. New conditions typically result in higher premiums, not a health insurance denial.
Individuals have been denied renewals from grandfathered plans in the past. If they wanted to apply for a new plan, though, they couldn’t be denied based on pre-existing conditions. Nevertheless, their premiums are most likely much higher under their new insurance plan.

Your annual income might be too high
Those applying for specific government-administered health insurance plans like Medicaid or Medicare can be rejected if their income is more than a certain amount. How much income residents can have and still qualify for these plans depends on various factors.
A sliding scale increases or decreases depending on how many minors are in the family. For instance, a family with three kids can earn more capital and still qualify for medical care over one with only one child. Is this fair?… You tell us!
The base numbers on the scale change each year. So families are urged to check this information regularly.
Incorrect information on a previous tax return
Another reason applicants can be met with health insurance denial is having false information on their prior tax returns. This reason may apply to people applying for Medicaid, Medicare, or plans from the health insurance marketplace.
In the past, some applicants faked their tax returns. Then, they chose to apply for a government subsidy on a plan from a health insurance marketplace. Therefore, they qualify for Medicare or Medicaid.
Those caught doing this can face a penalty or are banned from applying for a government plan for the remainder of their lives.
Those with a history of risky behavior
Those who have a history of medically risky behavior, like drinking alcohol in excess or smoking, may result in health insurance denial.
Smoking and drinking aren’t considered to be pre-existing conditions and, as such, aren’t covered under the provision that prevents insurers from rejecting someone due to a pre-existing condition.
An applicant with lung cancer as a result of cirrhosis from drinking or smoking can’t be denied based on their medical condition. However, they can be rejected based on their behavior.
Some health insurance advocates have made the case that individuals shouldn’t be dismissed for risky behaviors, but this law isn’t currently applicable.
COBRA Coverage can be denied for termination from a job
COBRA coverage refers to continuing health insurance benefits after an employee has been laid off. Former employees who chose to quit or were fired aren’t usually eligible for COBRA.
Someone applying for COBRA coverage after they’ve been released from a contract may also see their application denied. But exceptions do exist. For example, if the applicant has been wrongfully terminated, they could be eligible for COBRA coverage.
However, they will most likely have to prove that the dismissal was wrongful in a court of law.
What can a person do about health insurance denial?
If your health plan denies your claim for a service you’ve already obtained or denies a pre-authorization request, getting a health insurance denial is frustrating. But that denial doesn’t mean you can’t have that particular healthcare service.
Rather, it means that your insurer won’t pay for the service or that you need to appeal the judgment and potentially have it covered if your appeal is victorious.
If you’re willing to pay for the treatment out-of-pocket, you’ll likely be able to have the healthcare service without any further delays. If you can’t afford to pay out-of-pocket, you should look into the cause of the rejection to see if you can overturn it.
This process is called appealing a denial, and it can be accomplished in response to a previous authorization denial or the denial of a post-service claim. Non-grandfathered health plans have a specific procedure for appealing denials, which the Affordable Care Act codified.
The appeals process will be outlined in the report you receive when you’re notified that your claim or pre-authorization request has been rejected. Be sure you carefully follow the appeals process for your health plan.
Keep good records of each step you’ve taken, when you took them, and who you spoke with if you’re doing things on the phone. In most cases, your healthcare professional will also be closely involved in the appeals process.
They will take care of a good chunk of the insurance’s required documentation. If you can’t resolve the issue by working internally within your health plan, you can request an external review of the denial.
That means a government agency or neutral third party will review your claim denial. Note: There’s no guaranteed access to an external review if your plan is grandfathered. But the plan may still voluntarily offer this.
We hope this article on health insurance denials has been helpful. For some more information on this matter we highly recommend checking out this fantastic read from Amazon: Denials, Appeals & Adjustments: A Step by Step Guide to Handling Denied Medical Claims
Meanwhile, Easy Seniors Club is here for all your golden years needs! So on that note, we think you should also read: Support Your Brain Health: 12 Habits to Cultivate at 55 for a Sharp Mind at 85